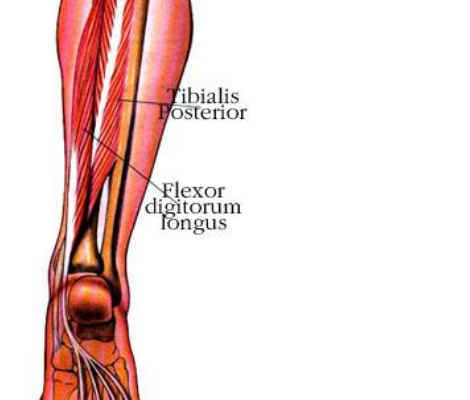
Reducing Spring Overuse Injuries: A Closer Look at Posterior Tibilias
Warmer spring temperatures and upcoming races mean longer runs and an increased risk of overuse injuries. Spring is common time for overuse injuries to the tibialis posterior muscle as it’s function in vital to efficient running. The…

Running Analysis to Improve Efficiency
by
John Fiore, PT
The strongest predictors of running injury include a prior history of running injury, running throughout the year without a break, and a rapid increase in running mileage of >10% per week (Br J Sports Med 2007). Identifying…

Static Versus Dynamic Stretching
(Should runners stretch and if so how?)
John Fiore, PT
www.sapphirept.com
Confusion and controversy exists regarding the proper way for runners to stretch. Some runners stretch regularly while some never stretch at all. Stretching confusion…

Calf Strength and Performance in the Master's Runner
Addressing Age-Related Calf Weakness
An average weekend in Missoula, Montana confirms the fact that 30 million people ran at least 50 days annually in the United States in 2012-2013. Running efficiently and injury-free, however, is more elusive.…

Sapphire PT Presentation at RE November 15th
Join Sapphire Physical Therapy on Wednesday, November 15 at 6:30 pm in the Runners Edge basement for an informative presentation. The presentation will focus on how impact loading rates during running relate to injury risk and discuss ways to…

The Drive Behind Achieving Goals: What Motivates us through Success and Failures
by John Fiore, PT
Sapphire Physical Therapy
November is a good month to reflect on the past year. As runners, this season reminds us how important it is to be thankful for our experiences and challenges in 2017. In order to set realistic running…


