Posts
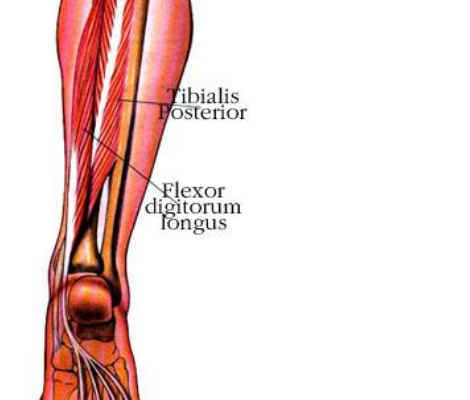
Reducing Spring Overuse Injuries: A Closer Look at Posterior Tibilias
Warmer spring temperatures and upcoming races mean longer runs and an increased risk of overuse injuries. Spring is common time for overuse injuries to the tibialis posterior muscle as it’s function in vital to efficient running. The…
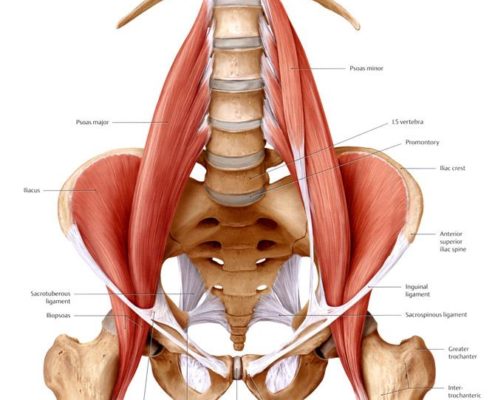
How Sitting Can Increase Injury Risk
by John Fiore, PT
Runners are well aware of the importance of strength training to reduce injury risk. Even the most specific strengthening program will fail to produce results, however, if compensatory movement patterns are not addressed.…


