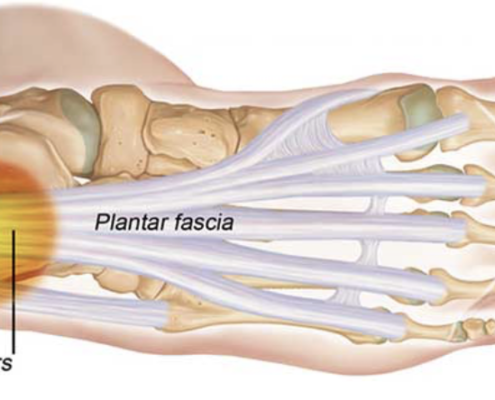
Understanding and Treating Plantar Fasciitis in Runners
Understanding and Treating Plantar Fasciitis in Runners
John Fiore, PT
Missoula area trails are in prime condition and the snow is melting in the high country. We are entering the season of running utopia in Western Montana and runners are…

The Mystery of Chronically Tight Hip Flexors
The Mystery of Chronically Tight Hip Flexors
Spring running miles are ramping up and as the ice melts our strides are opening up as well. There is a very good chance that you have felt or been told, you have “tight hip flexors.” Listening…

Staying active and fit during middle-age and beyond
John Fiore, PT
Background
Ten years ago, I wrote an article titled Running in Your Fifties and Beyond. Ten years later, and hopefully wiser, I will share the latest tips and research to decrease the myth and mystery of how to stay active and…

Utilizing Cross Training for Winter Running Training
By: Andrew Traver, PT, DPT
With summer running events looming, some runners may be initiating the early stages of their offseason training programs. Proper preparation is key for those who are expecting to participate in a running event(s),…

How to Reduce Running Injuries in 2023
By: John Fiore, PT
Winter in Montana can be a challenging time for runners in Montana. Winter is an excellent time to reflect on the past year and set realistic goals for the coming year. Winter in the time for runners to follow a solid…

Here’s why you keep getting injured, according to a physical therapist
Today, the hill feels easier to climb. I step and press firmly into the rain-saturated dirt and raise myself one step closer to the horizon line, my heels lifted. The springs at the back of my legs are loaded and ready…


