Understanding and Treating Plantar Fasciitis in Runners
John Fiore, PT
Missoula area trails are in prime condition and the snow is melting in the high country. We are entering the season of running utopia in Western Montana and runners are ramping up their weekly mileage in preparation for local and regional races on the roads and trails. Foot injuries are among the most prevalent location of running injuries. A dramatic increase in mileage without adequate foot and ankle strength greatly increases the risk of foot injuries such as plantar fasciitis. Understanding a bit about the structure and function of the foot is the first step in treatment and prevention of plantar fasciitis. The human foot is an under appreciated marvel. It is easy to take the foot for granted until foot pain occurs. The human foot is comprised of 28 bones and their associated ligaments, tendons, and muscles. While human feet have evolved to support upright walking (bipedal gait) and running, the repetitive impact of running, decreased foot and ankle strength, joint stiffness, and training errors may lead to foot pain. Plantar fasciopathy is a prevalent running injury as most of us increase our running mileage too quickly in the spring and summer. This article will focus on the plantar aspect of the foot. The plantar fascia plays a large role in the Windlass Mechanism which improves intrinsic foot support and contributes to our ability to run and hike efficiently. 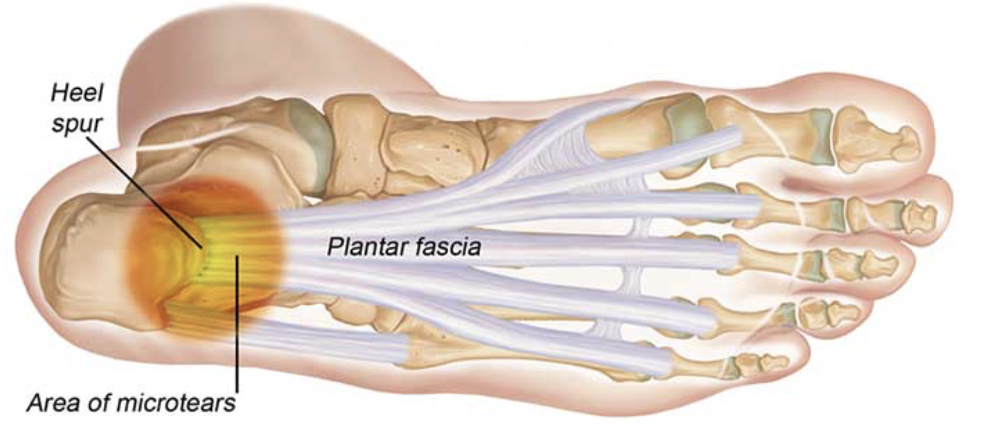
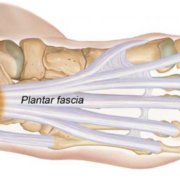
The plantar fascia is a thick fibrous band of connective tissue which runs from the front of the calcaneus (heel bone) to the base of the toes. It acts as a last resort to stabilize the longitudinal arch of the foot. Characterized by pain in the heel region of the arch of the foot, plantar fasciitis is the most common cause of heel pain requiring medical care. It is estimated that 1 in 10 people will develop plantar fasciitis in their lifetime, resulting in one million medical visit annually. Because plantar fasciitis often becomes a chronic condition, understanding the causes and proven treatment options will lead to effective resolution.
Plantar fasciopathy is a more accurate term to describe heel and arch pain as it includes the inflammatory condition (plantar fasciitis), and degenerative condition (plantar fasciosis) of the plantar fascia. Plantar fasciitis occurs when the thick, fibrous plantar fascia becomes inflamed due to trauma, poor foot strength, repetitive arch strain, or faulty foot-ankle biomechanics. Plantar fasciosis describes the non-inflamed degenerative state of the plantar fascia due to repetitive stress and chronic soreness.
Diagnosing plantar fasciitis involves palpating its attachment on the front of the calcaneus (heel bone). Pain is experienced during prolonged standing, running, descending stairs, and most notably upon rising and walking across the floor first thing in the morning. Additional causes of heel and plantar pain to be ruled out by your physician or physical therapist include bone stress reaction, stress fracture, localized nerve entrapment, and lumbar S1 radiculopathy. Predisposing factors to plantar fasciitis include repetitive impact (distance running,
jumping sports), rapid increase in activity level or mileage, poor intrinsic foot-ankle support, poor running biomechanics, and obesity (BMI >30).
Effective treatment of plantar fasciopathy takes place over four phases:
Acute Pain Phase: During the acute pain phase, pain must be reduced by avoiding running, hopping, and prolonged standing. Providing additional support through taping, use of anti-inflammatories (if inflammation is present), and reducing impact through gel heel cups and comfortable footwear may be part of the acute pain phase of rehabilitation. Isometric toe flexor exercises, active stretching techniques for the plantar fascia and gastroc-soleus muscle group will improve foot and ankle mobility and function.
Gradual Loading Phase: Manual physical therapy, progressive lower leg and ankle resisted exercises are added during the gradual loading phase. Underlying hip, glut, and core weaknesses must be addressed as well. Gradual plantar fascia loading exercises begin with double leg heel raises followed single leg heel raises as tolerated. Proper technique is crucial to begin to build loading and weight bearing tolerance.
Heavy Loading Phase: Once single leg heel raises are tolerated pain-free, a barefoot modified (towel roll beneath toes) single leg calf raise progression is commenced. The Rathleff loading program (Rathleff et al 2014) continues to add resistance to single leg heel raise progressions over four weeks, building eccentric strength and tension tolerance. Running and hiking are reintroduced upon successful completion of the Rathleff program. For runners, a 2D video running analysis is vital to insure proper running biomechanics to reduce re-injury.
Orthotics and Shoes: Proper running shoes are vital for comfort and support. Shoe preference is a personal choice, but selecting a shoe based on your foot structure, foot strike pattern, running terrain, and mileage is important. The shoe experts at Runners Edge can assist you in selecting the right shoe for you. Orthotics are very effective in treating persistent plantar fasciitis and plantar fasciosis. Sapphire Physical Therapy fabricates custom foot orthotics for runners on-site for optimal results. A custom orthotic with a slight heel lift, supportive heel cup to decrease excessive rear foot motion (pronation-supination), and an adequate arch support and rocker are key orthotic components when treating plantar fasciitis and plantar fasciopathy. Although custom orthotics do not take the place of strengthening and realistic training mileage and loads, they do improve the support and mechanics of the foot in weight bearing. Learn more about our custom orthotics at https://www.sapphirephysicaltherapy.com/custom-foot-orthotics
A successful return to distance running requires proper foot and ankle support, foot intrinsic strength, and lower leg mobility and strengthening exercises. Proper footwear, insoles or custom orthotics, adequate recovery following exercise, and gradual, targeted increases in training loads will help keep plantar fasciitis-fasciopathy and other foot issues from returning. The experts at Sapphire Physical Therapy can evaluate your running gait, detect underlying strength issues, and develop a foot injury prevention and treatment program to meet your individual needs. Call Sapphire Physical Therapy or learn more at www.sapphirephysicaltherapy.com and don’t let your feet keep you from meeting your 2023 running and adventure goals.
John Fiore, PT
References:
Riddle DL, Pulisic M, Pidcoe P, Johnson RE. Risk factors for plantar fasciitis: a matched case-control study. J Bone Joint Surg Am. 2003:85-A:872-7
Riddle DL, Schappert SM. Volume of ambulatory care visits and patterns of care for patients diagnosed with plantar fasciitis: a national study of medical doctors. Foot Ankle Int. 2004 May. 25(5):303-10
DiGiovanni BF, Nawoczenski DA, Lintal ME, et al. Tissue-specific plantar fascia stretching exercise enhances outcomes in patients with chronic heel pain. J Bone Joint Surg Am 2003:85-A(7):1270-7
Rathleff MS, Molgaard CM, Fredberg U, et al. High-load strength training improves outcome in patients with plantar fasciitis. Scand J Med Sci Spor 2014
Photo: www.semanticscholar.org