Posts

The Time to Improve Foot Function is Now
By: John Fiore, PT, owner of Sapphire Physical Therapy
The function of the foot
The human foot is an evolutionary marvel. The human foot contains twenty-six bones, thirty-three joints, and one-hundred ligaments, muscles, and tendons.…

Sapphire PT Corner: Bone Stress Injuries and RED-S in Female Runners
Evie Tate, PT, DPT
Sapphire Physical Therapy
Bone stress injuries (BSI) or “stress fractures” are one of the more common running-related injuries seen in female runners (1,2). These injuries occur when our bones are broken down faster…
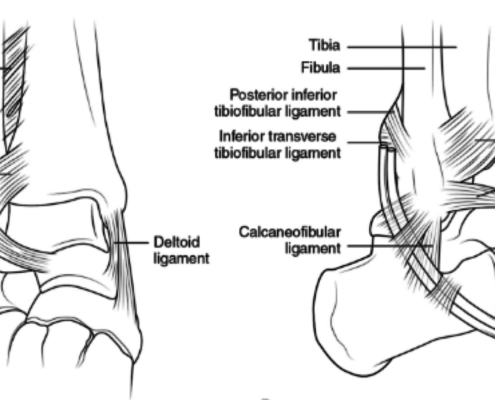
Ankle sprains are one of the most common injuries experience by trail and mountain runners due to the steep and uneven terrain. Ankle sprains, however, are not all alike. In last month’s Runners Edge Newsletter, lateral ankle sprains were…

Calf Strength and Performance in the Master's Runner
Addressing Age-Related Calf Weakness
An average weekend in Missoula, Montana confirms the fact that 30 million people ran at least 50 days annually in the United States in 2012-2013. Running efficiently and injury-free, however, is more elusive.…
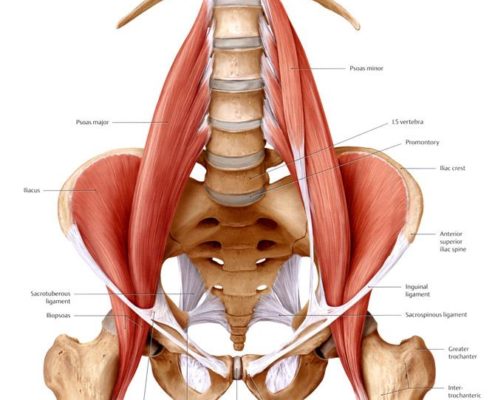
How Sitting Can Increase Injury Risk
by John Fiore, PT
Runners are well aware of the importance of strength training to reduce injury risk. Even the most specific strengthening program will fail to produce results, however, if compensatory movement patterns are not addressed.…

Downhill Running Form and Training Techniques
Downhill Running Form and Training Techniques
John Fiore, PT
The challenges of running uphill are addressed through uphill interval training and techniques specific to climbing. Downhill running, however, is often a forgotten aspect of training.…


