Ankle sprains are one of the most common injuries experience by trail and mountain runners due to the steep and uneven terrain. Ankle sprains, however, are not all alike. In last month’s Runners Edge Newsletter, lateral ankle sprains were discussed. Most of the athletes treated for ankle sprains at Sapphire Physical Therapy participate in activities which involve running, jumping, sprinting, skating, or sliding into base. Many of these individuals present with some degree of high ankle sprain. This vague and general term warrants explanation for effective treatment and timely return to activities.
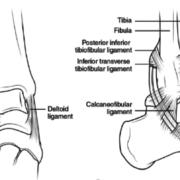
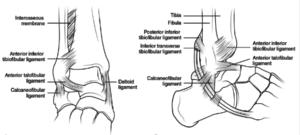
The anatomy of a high ankle sprain involves four main ankle ligaments (see illustration) plus one often forgotten structure: the syndesmosis or interosseous ligament. The syndesmosis ligament provides stability for the movement of the tibia and fibula as a unit over the talus bone of the ankle. Normal widening or splaying of the tibia and fibula is only 1 mm thanks to the syndesmosis ligament.
*Photo credit: Browner B, Jupiter J, Levine A, Trafton P: Skeletal Trauma: Fractures, Dislocations, Ligamentous Injuries, ed 3. Philadelphia, PA, Saunders, 2003, vol 2, p 2307-2374.)
High ankle sprains are familiar to runners as well as soccer, lacrosse, and hockey players. What makes high ankle sprains difficult to diagnose and treat is the fact that most ankle sprains are minor and heal following several days of rest and conservative treatment. When the syndesmosis ligament is strained, however, pain, stiffness, and poor weighe bearing tolerance persists. When the syndesmosis ligament complex is suspected due to a high ankle sprain, specific testing should be conducted for effective treatment.
The syndesmosis ligament complex is often strained secondary to high impact, forced dorsiflexion (foot bent upward) combined with an eversion (inside of foot rolls outward) sprain. A sudden, high velocity ankle roll with impact sufficient to force the foot in an upward motion which increases the widening or splaying between the tibia and fibula bones. The deltoid ligament may or may not be involved in a high ankle eversion sprain as well. Swelling may or may not be present, and syndesmotic sprains characteristically do not get better on their own. Athletes commonly express frustration due to the fact that rest, ice, elevation, and an over-the-counter ankle brace did not allow them to return to running or sport. Sources place the frequency of ankle syndesmosis injuries at 1% to18% of all ankle sprains. In athletes and runners, however, the incidence increases to 12% to 32%.
Fractures should be ruled out in the case of a high ankle sprain. If swelling subsides within two days and weight bearing becomes pain-free, then an X-ray may not be indicated. If symptoms of swelling, pain, and difficulty weight bearing persist, then an X-ray is indicated. Magnetic resonance imaging (MRI) may be indicated if a syndesmotic injury is suspected. Research has shown X-rays to be less accurate (44% to 58% specificity) than MRI (nearly 100% specificity) in diagnosing a syndesmosis ankle sprain component. The degree of tibia-fibula gapping or splaying (positive when greater than 1 mm lateral subluxation or greater than 5 mm separation between the distal fibula and tibia) and the stability of the ankle (presence or absence of additional ankle sprains, stability, or fracture) will determine whether conservative treatment or surgery is the best course of action.
Treatment: Ankle inflammation reduction and rest, followed by progressive mobility and stability are necessary for proper ankle rehabilitation following an ankle sprain. If a fracture is present, then the treatment progression will occur secondary to fracture healing which is usually 6-8 weeks. A high ankle sprain involving the syndesmosis ligament requires stabilization for pain-free weight bearing activities prior to returning to running and sports. If the correct conservative treatment measures fail, surgery may be necessary. The treatment techniques described below, therefore, should be done only after a thorough evaluation including clinical and diagnostic testing.
Taping: Some degree of syndesmosis ligament stabilization is possible with taping. A physical therapist with experience treating high ankle sprains should apply the taping techniques described below:
The distal tibia and fibula must be taped circumferentially with a strong, non-stretch, durable tape. I use a base tape to protect the skin followed by strips of Leukotape. Pain reduction should be >50% with tape applied to allow for walking without a limp. Return to activities and exercise should occur only if taping provides pain-free weight bearing. I also utilize the Mulligan high ankle sprain taping technique to stabilize the lateral ankle ligaments and tibia-fibula joint.
Braces: A walking boot may be necessary to allow for early mobility following an ankle sprain. If pain is too great to allow for weight bearing without a walking boot one week following a high ankle sprain, diagnostic testing is warranted. A soft Velcro ankle brace (referred to as an ASO brace) will provide some ankle support but will not stabilize the syndesmosis ligament.
Range of motion, strength and balance: Pain-free ankle active range of motion is the necessary first step in treating a high ankle sprain. Once full pain-free motion is achieved, lower leg, foot, and hip strength must be evaluated and addressed. Restoring single leg balance and proprioception (positional body awareness) will reduce ankle sprain re-injury risk. Research has shown heightened ankle sprain risk in the presence of limited dorsiflexion range of motion, reduced proprioception, and decreased single leg standing balance. Restoring ankle range of motion and strength is followed by gradually adding in weight bearing static and dynamic exercises. Post-high ankle sprain rehab culminates with agility and balance drills specific to your sport or activity goals.
- Hunt KJ, Phisitkul P, Pirolo J, Amendola A. High Ankle Sprains and Syndesmotic Injuries in Athletes. JAAOS 2015 Nov;23(11):661-673.
- Mak MF, Gartner L, Pearce CJ. Management of syndesmosis injuries in the elite athlete. Foot Ankle Clin N Am. 2013;18(2):195–214.
- Waterman BR, Belmont PJ, Jr, Cameron KL, Svoboda SJ, Alitz CJ, Owens BD. Risk factors for syndesmotic and medial ankle sprain: role of sex, sport, and level of competition. Am J Sports Med. 2011;39(5):992–998.
- de-las-Heras Romero, J., Alvarez, A. M. L., Sanchez, F. M., Garcia, A. P., Porcel, P. A. G., Sarabia, R. V., & Torralba, M. H. (2017). Management of syndesmotic injuries of the ankle. EFORT Open Reviews, 2(9), 403–409. http://doi.org/10.1302/2058-5241.2.160084
- Vuurberg G, Hoorntje A, Wink LM, et al. Diagnosis, treatment and prevention of ankle sprains: update of an evidence-based clinical guideline Br J Sports Med 2018;52:956.