Posts

The Time to Improve Foot Function is Now
By: John Fiore, PT, owner of Sapphire Physical Therapy
The function of the foot
The human foot is an evolutionary marvel. The human foot contains twenty-six bones, thirty-three joints, and one-hundred ligaments, muscles, and tendons.…
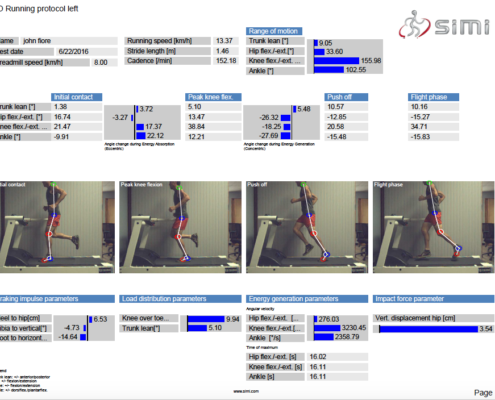
High Speed 2D Video Running Analysis
Injuries impact nearly 80% of all runners at some point (Br J Sports Med 2007). While some runners rarely miss a training run or race due to injury, many experience a variety of injuries and/or recurrent injuries. The key to effectively treating…

Training Consistency for Successful Distance Running
The roads and lower elevation trails around Missoula have melted after being snow-covered since mid-December. April 1st is the day fools like me test out our skiing fitness and ramp up our running mileage in preparation for early season…
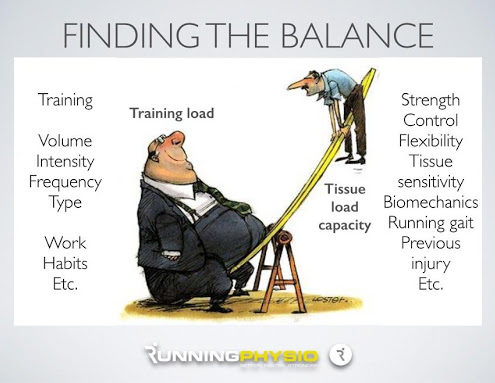
Winter Running and Training Tip: Reducing off season hamstring injury
By: John Fiore, PT
Sapphire Physical Therapy
The sun appeared today and the thermometer reached 40 degrees Fahrenheit (ed. note: this was written last week!). Warmer temperatures and sp ring racing commitments result in a rapid increase in…
Practical Winter Running Tip: Protecting Your Feet from Potential Traction Mishap
By John Fiore, PT
Sapphire Physical Therapy
Icy and snow-packed roads and trails synonymous with winter in Montana are here. While Missoula runners often trade running shoes for ski boots, January marks the beginning of training for the…

Proximal Hamstring Pain in Runners
By: John Fiore, PT
The hamstring is an important and complex muscle group used in running. While minor hamstring pulls and strains are fairly common in runners, proximal hamstring overuse injuries can be very debilitating. Repetitive micro-trauma…


